Fast-Track Approvals, Fewer Claim Delays
Accurate Insurance Verification & Prior Authorization Support for Healthcare Providers
At MediFunding Consulting , we simplify insurance processes for busy practices with reliable insurance verification services for medical offices and seamless prior authorization support for doctors . Our team ensures that eligibility, benefits, and coverage details are verified upfront, so your claims are accepted the first time and patients receive uninterrupted care.
Expert Insurance & Authorization Solutions
Clear Verifications. Fast Approvals. Smarter Workflow.
Denied claims and delayed authorizations can cost practices time, money, and patient satisfaction. With our outsourced insurance verification for clinics, we ensure all details are accurate before services are rendered. We identify whether prior authorizations are needed, submit requests promptly, and follow up until approval—saving your staff time and reducing the risk of revenue loss.
MediFunding Consulting is your trusted partner in eligibility checks, payer communication, and authorization tracking.
Our Streamlined Verification & Authorization Process
Insurance Eligibility & Benefits Verification
We confirm patient coverage details including co-pays, deductibles and benefit limits to minimize billing issues.
Coordination of Benefits (COB) Review
We identify and validate primary and secondary insurance payers to ensure accurate claim submission and payment.
Network Participation Check
We verify if your practice is in-network or out-of-network with the patient’s plan, helping avoid unexpected costs.
Prior Authorization Assessment
We determine which procedures, services, or medications require pre-approval based on payer rules.
Authorization Request Submission
Our team submits complete prior authorization requests through the correct channels with all required documentation.
Status Monitoring & Follow-Up
We continuously track authorization status, provide timely updates, and fast-track urgent cases to prevent delays.
Payer Communication Management
We handle all correspondence with insurance companies to streamline approvals and reduce administrative burden on your staff.
Denial Prevention & Resolution
We proactively address potential issues to reduce denials and resolve them swiftly if they occur.
Documentation & Compliance Support
We maintain detailed records for all verifications and authorizations, supporting payer compliance and audit readiness.
Why Choose MediFunding Consulting?
Specialized Support for Clinics
We provide customized insurance verification services that reduce admin workload and accelerate patient onboarding.
Comprehensive, End to End Solutions
From eligibility verification to prior authorizations, we manage the entire process seamlessly and efficiently.
Higher Claim Acceptance Rates
Our thorough verification process results in cleaner claims, minimizing denials and speeding up reimbursements.
Direct Payer Communication
We proactively engage with insurers to resolve issues quickly and prevent delays caused by miscommunication.
Flexible & Scalable Services
Whether you are a solo provider or a large clinic, our solutions scale to fit your needs and integrate with your workflow.
Dedicated Expertise & Compliance
Our experienced team stays current on payer guidelines and ensures your practice remains compliant and audit-ready.
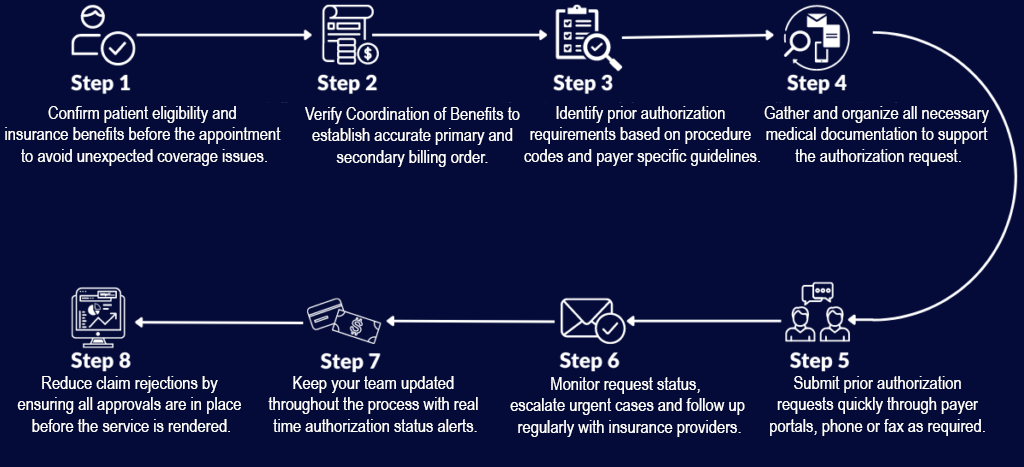
Step-by-Step Insurance Verification Process
Our streamlined process helps ensure fewer denials, faster approvals and smoother billing so your team can focus more on patient care.
Additional Verification & Authorization Services

Real-Time Insurance Verification
Instant coverage checks through payer systems.

Medication Prior Authorization
Faster approvals for specialty and high-cost drugs.

Referral Coordination
Verify and document necessary referrals to avoid claim denials.

Retro Authorization Assistance
Help securing post-service approvals when required.

Specialty Procedure Review
Confirm benefits and pre-approvals for advanced diagnostics or therapies.

Out-of-Network Billing Assistance
Provide clarity on patient responsibility and reimbursement expectations.
Ready to Improve Authorization Efficiency?
Partner with MediFunding Consulting to reduce denials, increase payment speed and free up your front office team. Whether you need insurance verification services for medical offices or reliable prior authorization support for doctors, we are here to help.
Contact us today for a free consultation and discover how outsourcing these critical services can elevate your practice.
